Emergency care across Europe is under growing pressure. Long waits, corridor care, and overstretched teams are no longer unusual in emergency departments, but part of everyday reality. Clinicians must assess patients quickly, prioritise care safely, and document decisions, often while working across multiple systems.
Digital tools cannot solve these structural challenges on their own. They do not create capacity or replace missing staff. However, the way clinical information is captured, shared, and reused can make a meaningful difference in how teams work under pressure.
In this article, we explore where interoperable digital tools can realistically support emergency care workflows, and how Better is contributing to this by introducing a new Emergency care bundle in Better Marketplace, designed to support everyday clinical work within today’s constraints.
Growing pressures in emergency care
Emergency care is one of the most demanding areas of modern healthcare. Clinicians work in fast-paced, high-pressure settings, where they must assess patients quickly, prioritise care, and document decisions clearly, often while managing high patient volumes and limited resources. When demand exceeds capacity, one of the clearest signs of this strain is reflected in long waiting times for patients.
These prolonged waits are nothing new and are no longer an exception. National reports and media investigations increasingly describe long waiting times as a defining feature of emergency care across Europe. According to The Guardian, in the UK alone, more than one million older people each year wait longer than 12 hours in A&E (Accident and Emergency), many of them treated on trolleys in corridors. In Portugal, some hospital emergency departments have reported waiting times exceeding 30 hours, driven by staff shortages and closed units, as reported by Euronews. In Slovenia, reports from UKC Ljubljana describe elderly patients waiting more than 10 to 20 hours for admission, often unable to access basic care needs while waiting (RTV Slovenija).
These examples come from different healthcare systems, yet the underlying challenges are strikingly similar: shortages of beds, limited professional staff, and steadily increasing demand. It is important to be clear that interoperable digital tools do not solve these structural problems on their own. They cannot create additional hospital beds or replace missing clinicians, and technical interoperability is not a silver bullet for overcrowded emergency departments.
What it can do, however, is reduce administrative burden and help teams work more efficiently within these constraints.
Where digital tools can help make a difference
When emergency departments are under extreme pressure, inefficiencies become costly. Clinicians spend time re-entering data, switching between systems, recalculating scores, or trying to gain an overview of patient status or bed availability. Interoperable tools can reduce this friction by enabling:
✅ Faster access to structured clinical data across systems
✅ Real-time sharing of observations, assessments, and scores
✅ Better situational awareness of patient acuity and resource use
✅ More consistent and timely decision-making at the point of care
This does not shorten queues overnight, but it can speed up individual patient journeys, reduce duplication, and help teams prioritise care more safely when demand exceeds capacity.
What the new Emergency care bundle on Better Marketplace brings
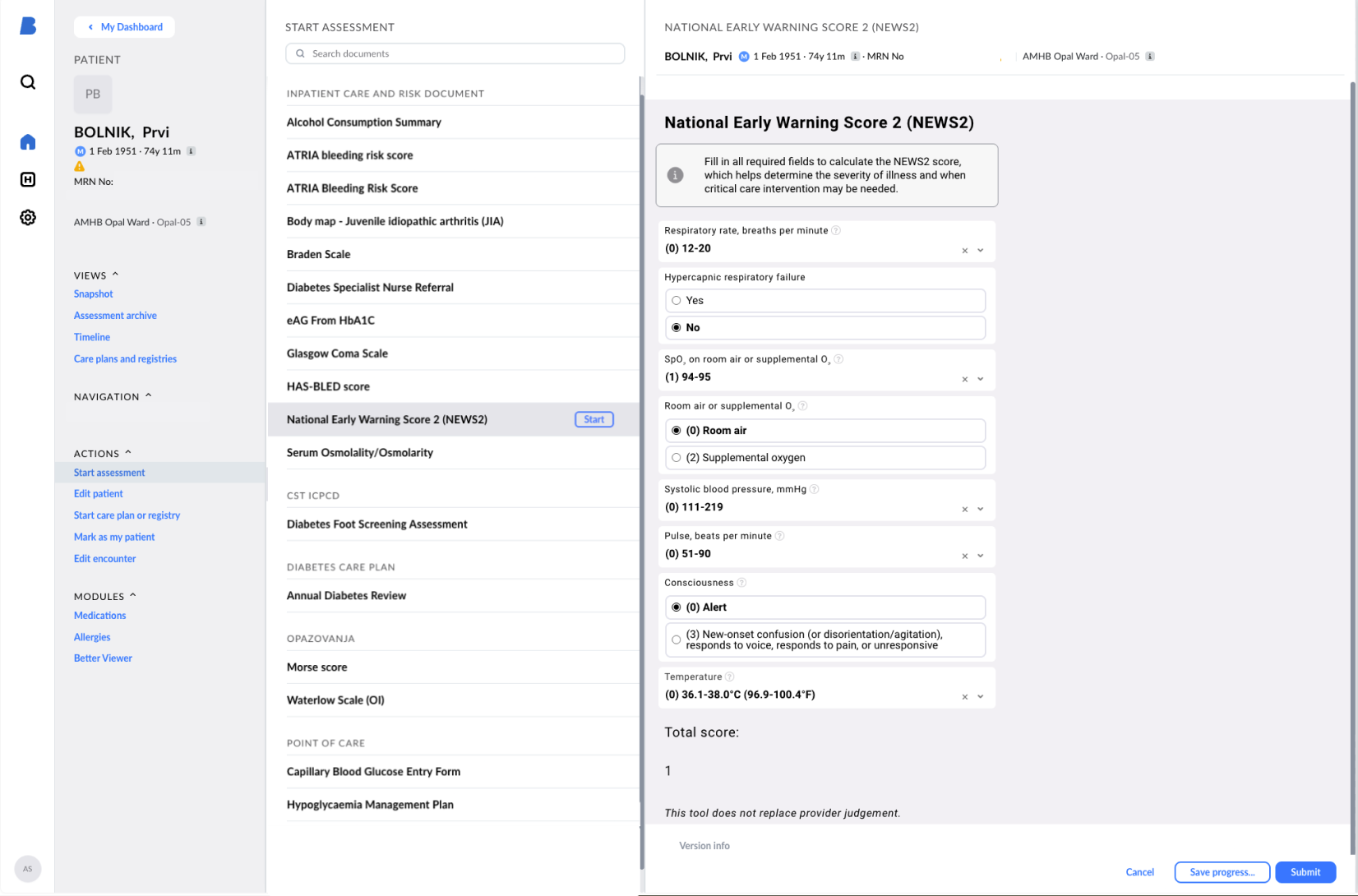
The new tools in the Emergency care bundle available for free in Better Marketplace focus on exactly these high-pressure moments. It brings together a set of widely used, evidence-based tools that support triage, risk stratification, and early detection of deterioration, including:
✅ Early warning and deterioration: NEWS2, qSOFA, SOFA
✅ Neurological and cognitive assessment: Glasgow Coma Scale, RASS, 4AT (delirium screening)
✅ Acute risk stratification: HEART score, ABCD² score for TIA, CHA₂DS₂-VASc
✅ Infection and respiratory assessment: CURB-65, CRB-65
✅ Acute abdominal assessment: Alvarado score, AIR score
✅ Supporting calculations: BMI, BSA, ideal and adjusted body weight, creatinine clearance
Some of these tools guide critical decisions about admission, escalation, or discharge. Others, such as BMI, BSA, or renal function calculations, quietly underpin safe dosing and everyday clinical decisions. Additional tools will be added over time to further support routine assessment and decision-making across emergency care workflows.
Built using openEHR and designed for reuse, these tools can be integrated directly into clinical workflows, allowing data to be captured once and reused across systems. At the same time, they also serve as a practical learning resource: each tool can be explored as a concrete example of how to structure, model, and implement your own clinical tools, helping teams understand how openEHR-based components are built and reused in practice.
Interoperability to support efficiency
As said, emergency care systems across Europe are under growing strain. Long waiting times, corridor care, and staff exhaustion are no longer isolated issues, but signs of bigger structural pressures that technology alone cannot resolve. Still, in settings where time, attention, and resources are stretched thin, even small improvements in how patient data is captured, shared, and reused can make a significant difference.
Interoperable digital tools can help emergency teams spend less time navigating systems and more time focusing on patients. By supporting quicker assessments, clearer prioritisation, and better coordination across departments and organisations, they help reduce friction in everyday work. Over time, they also contribute to more consistent, structured data, which is necessary for understanding bottlenecks, planning capacity, and improving services at a wider system level.
The work we put into this Emergency care bundle is not about fixing emergency care overnight. It is about supporting healthcare and clinicians with practical tools that fit into their workflows and help ensure that clinical information follows the patient, rather than being lost between systems. We believe that as the pressure on healthcare continues to grow, this kind of support is becoming a necessary part of how care is delivered.
Conclusion
At Better, we continuously develop new ways to support healthcare teams and improve care delivery. After this addition of emergency care tools to the Marketplace, we are expanding this work further, with the next clinical specialisation already on the horizon.
Sources
- The Guardian. “More than 1m older people in England waited 12 hours in A&E last year.” 6 May 2025. Available from: https://www.theguardian.com/society/2025/may/06/more-than-1m-older-people-england-waited-12-hours-ae-last-year
- Euronews. “Portuguese hospitals hang by a thread with closed A&E departments, lack of staff and long queues.” 13 February 2025. Available from: https://www.euronews.com/2025/02/13/portuguese-hospitals-hang-by-a-thread-with-closed-ae-departments-lack-of-staff-and-long-qu
- RTV Slovenija. “Dolge čakalne dobe v UKC Ljubljana: za sprejem v bolnišnico treba čakati tudi več kot 10 ur.” 2025. Available from: https://www.rtvslo.si/zdravje/dolge-cakalne-dobe-v-ukc-ju-ljubljana-za-sprejem-v-bolnisnico-treba-cakati-tudi-vec-kot-10-ur/728590