Every November, World Diabetes Day reminds us not only of the scale of the challenge, but also of our shared responsibility to act with clarity and purpose. Type 2 diabetes is not an isolated diagnosis. It is a condition interwoven with hypertension, obesity, cardiovascular disease and a growing list of long-term comorbidities that complicate every prescription, every review and every follow-up.
Clinicians have seen this first-hand. Patients who start with one or two medicines often leave the pharmacy with six or seven. Notes and results scatter across systems. Each specialist means well, yet their collective effort can feel fragmented. In this complexity, it’s easy to lose sight of prevention and structured review, the quiet, systematic work that prevents crises before they happen.
But there is hope in the tools we build together. Not miracle drugs, but digital foundations that bring coherence back to care.
The growing burden of type 2 diabetes
Globally, diabetes rates have quadrupled in just four decades. According to the World Health Organization, nearly one in seven adults now lives with the condition, with type 2 accounting for more than 80 % of cases (1). The International Diabetes Federation predicts these numbers will continue to climb throughout the next decade (2).
Behind this statistic lies a familiar story: a gradual rise in blood glucose, weight, blood pressure, and lipids, followed by medication upon medication. In some studies, people with diabetes take an average of five medicines at the same time. The consequences are real: drug interactions, poor adherence, hospital admissions, and a growing sense that healthcare is something done to patients rather than with them.
For clinicians, this creates what could be described as a “care fragmentation loop.” They are urged to follow disease-specific guidelines, yet the patients rarely live with only one condition. The result is a heavy cognitive burden, repetitive data entry, and a constant risk of overlooking the early signs that prevention is still possible.
What clinicians need most
When we speak honestly about daily practice, three needs appear time and again:
- Early risk detection. Simple, validated tools to identify those moving towards diabetes long before HbA1c confirms it.
- Structured, reusable data. Consistent recording of key risk factors such as weight, waist measurement, blood pressure, and medication lists in formats that can be reused rather than retyped.
- Decision support at the point of care. Tools that fit naturally into the workflow, not as separate portals or static PDFs, but as focused, meaningful modules that help clinicians act in the moment.
These are not grand ambitions. They are the quiet foundations of safer, more personalised care.
Closing the gaps in multimorbid diabetes care with low-code and openEHR
Digital technology is sometimes criticised for placing more screens between clinicians and patients. Yet, when designed well, it can do the opposite: simplify complexity and bring the focus back to the person in front of us.
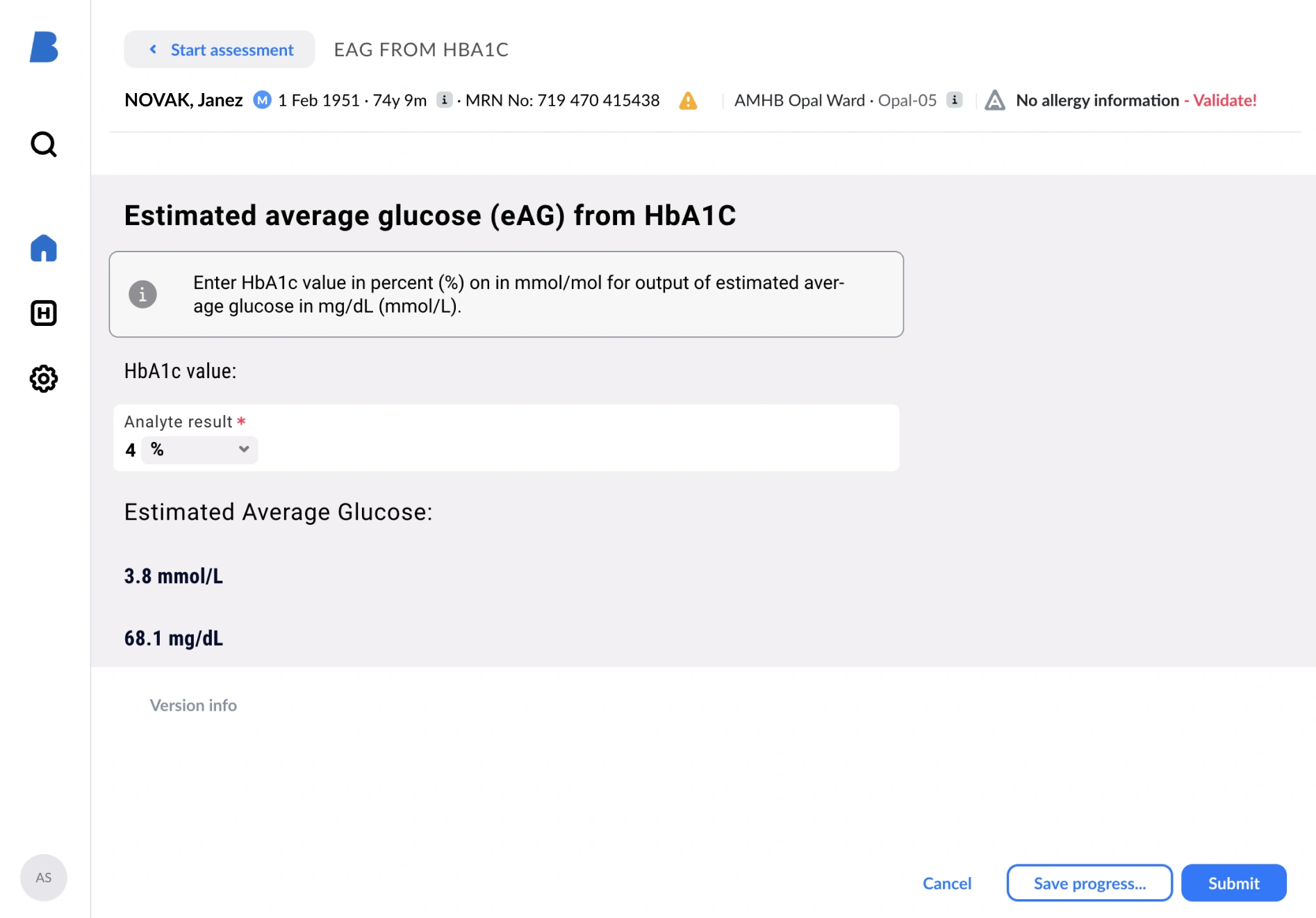
This is where low-code clinical tools built on openEHR standards make a real difference. Low-code platforms enable clinicians, informaticians, and developers to co-create tools quickly, without lengthy software cycles. A new diabetes risk form, a medication review widget, or a dashboard showing HbA1c and lipid trends can be designed, tested, and deployed in weeks rather than months.
openEHR ensures that every data point captured, from waist circumference to treatment goals, follows an agreed structure. This makes the information reusable, computable, and shareable across systems, settings, and even countries. Together, they help close the gap between insight and action.
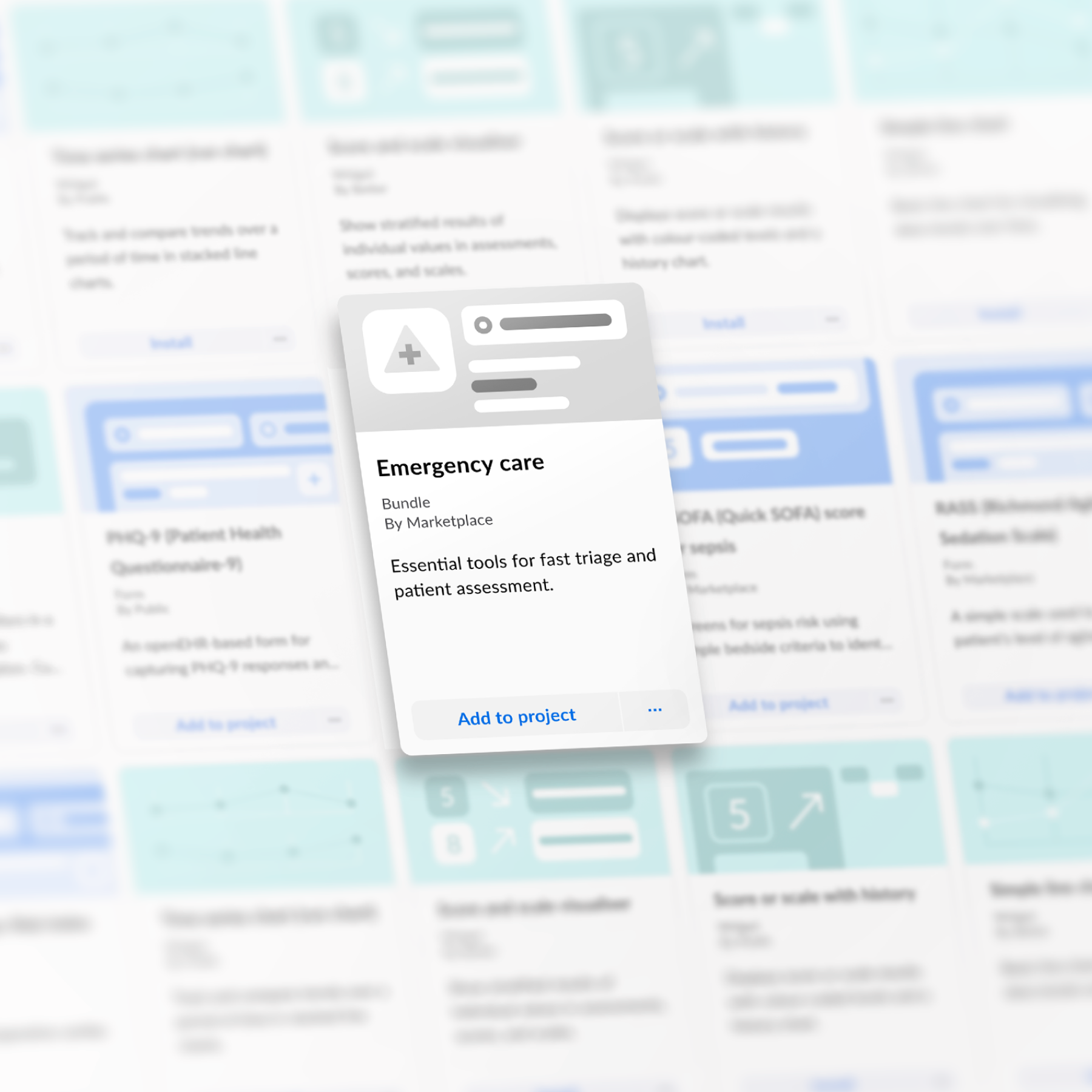
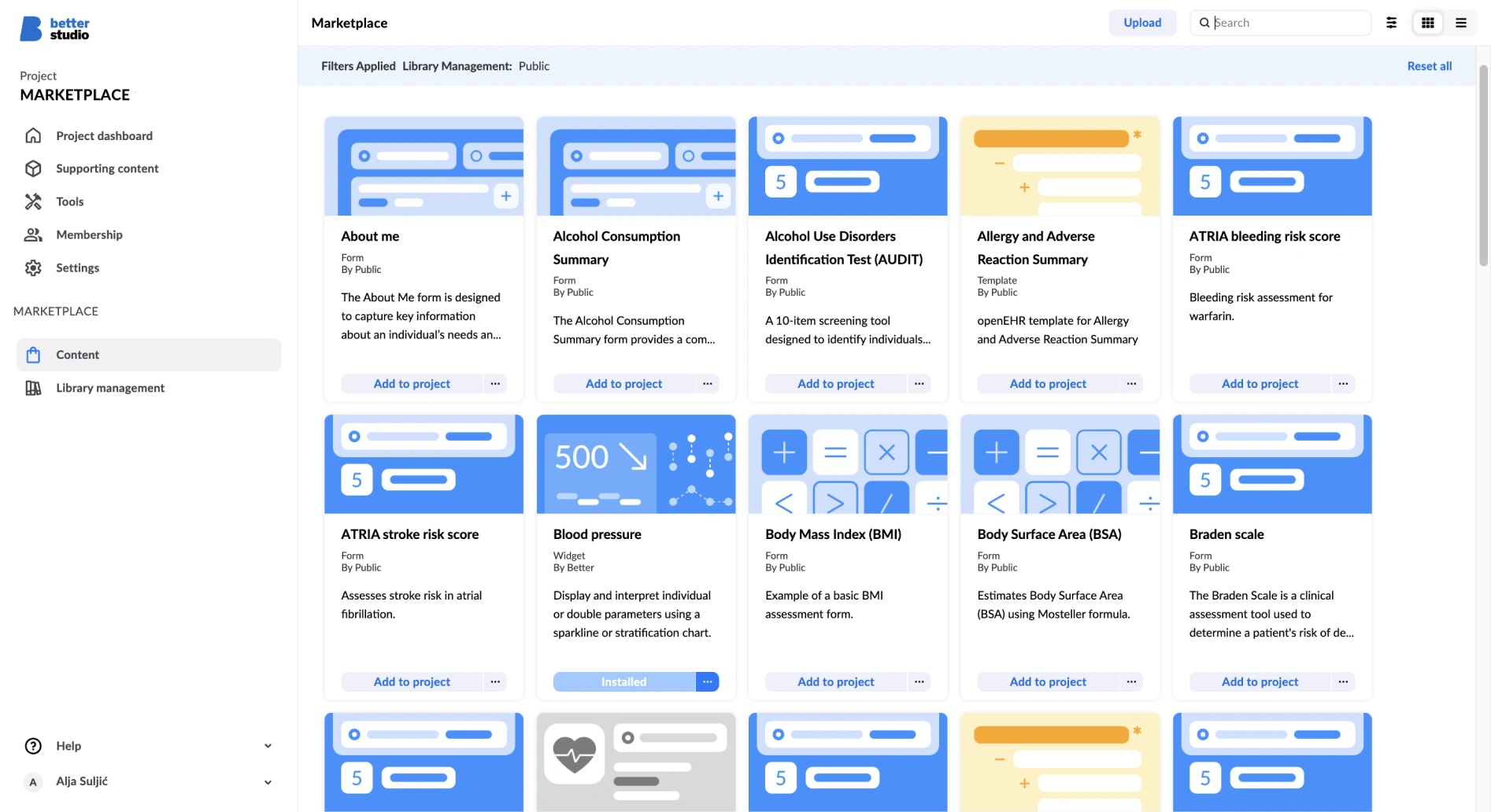
And this is exactly why at Better we have published a freely available Endocrinology bundle on Better Marketplace, a collection of ready-to-use clinical tools for patient care that can be embedded directly into electronic workflows. The bundle includes validated calculators, structured assessment forms, and reusable data models that support early risk detection, medication safety, and long-term monitoring.
In practice, the Endocrinology bundle brings together a set of ready-to-use clinical tools for metabolic and endocrine care. It includes calculators for calculated LDL, eAG from HbA1c, serum osmolality or osmolarity, BMI and BSA, as well as structured forms for waist and hip circumference with automated waist-to-hip ratio calculation, plus ideal and adjusted body weight. In addition, it features risk scores, such as FINDRISC score for quick assessment of ten-year risk of developing type 2 diabetes using simple lifestyle and anthropometric data. And this is only the beginning; more endocrinology content is already on its way.
From Better Studio to Better Marketplace: Scaling what works
At Better, this concept is evolving into a practical ecosystem.
Better Studio is where clinicians and partners design and build these low-code tools. Better Marketplace is where they share them, enabling others to adopt, adapt and extend what already works.
Instead of every hospital or health system starting from scratch, the Marketplace allows teams to reuse a tested diabetes risk score, integrate it into their local workflows and build upon it for their specific population. This not only saves time and resources, it also ensures consistency of data and accelerates innovation. A widget refined by one clinical team can immediately benefit another.
In this way, digital health becomes communal, a living library of shared knowledge and practice.
World Diabetes Day: A call to collaborate
This World Diabetes Day, the theme is action, not just awareness. The future of chronic disease care will not hinge on a single discovery, but on a collective effort to standardise, share and reuse what works. By building low-code tools in open, interoperable formats, and by sharing them through a collaborative marketplace, we turn fragmented care into connected care
- For prevention, through risk-score calculators and early-screening workflows.
- For safety, through medication-review and polypharmacy-monitoring widgets.
- For collaboration, through open standards that let data travel, so patients do not have to repeat their story at every door.
We may not eliminate diabetes, but we can build systems that detect risk earlier, manage complexity more intelligently, and make every encounter count. The shift begins with clinicians shaping the tools they use, designing, sharing and improving them together.
It is, at heart, a simple proposition: care through structure, growth through reuse, community through collaboration. That is the spirit of World Diabetes Day, and the promise of digital health done right.
To start with Endocrinology bundle and other content on Better Marketplace, sign in to Better Studio first, then access Better Marketplace to discover our new integrated cardiology tools and enhance patient care.
Sources
- World Health Organization. “Diabetes – Fact sheet.” 10 November 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/diabetes
- International Diabetes Federation. IDF Diabetes Atlas, 10th edn. Brussels: IDF; 2021. Magliano DJ, et al. “Global picture.” In: Global, regional and national burden of diabetes from 1990 to 2021… (Supplement). NCBI Bookshelf. 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK581940/